Two years of the COVID-19 pandemic in Latin America and the Caribbean: reflections for advancing towards universal, comprehensive, sustainable and resilient health and social protection systems
Topic(s)
Analysis of the evolution of the pandemic clearly shows that the health crisis has not passed and that uncertainty remains. The prolonged crisis has highlighted not only the weaknesses of the region's health and social protection systems, but also the centrality of health for social and economic development.

Analysis of the evolution of the pandemic clearly shows that the health crisis has not passed and that uncertainty remains. The prolonged crisis has highlighted not only the weaknesses of the region's health and social protection systems, but also the centrality of health for social and economic development.
After the World Health Organization declared the coronavirus disease (COVID-19) a pandemic on 11 March 2020, the profound health and social crisis unleashed by the disease generated a severe deterioration in the living conditions of the population. Into the third year of the pandemic, the signs of recovery from the economic crisis that began to emerge in 2021 are projected to weaken in 2022.
Structural inequalities in Latin America and the Caribbean have made the region more vulnerable to the pandemic, in terms of both the number of cases and deaths from COVID-19. The document “Dos años de pandemia de COVID-19 en América Latina y el Caribe” provides evidence on how uneven impact of the pandemic has been across and within countries. It shows, for example, that excess mortality was higher in those countries with higher levels of poverty, extreme poverty (see figure 1) and informal labour markets. In this sense, the document discusses how the axes of the matrix of social inequality are closely related to the unequal impact of the pandemic, through the disparate distribution of the social determinants of health, and emphasizes the urgent need to articulate health and social protection systems in a much more joined up manner.
América Latina (17 países): exceso de mortalidad, según pobreza extrema, 2020-2021
(En muertes por cada 100.000 habitantes y porcentajes)
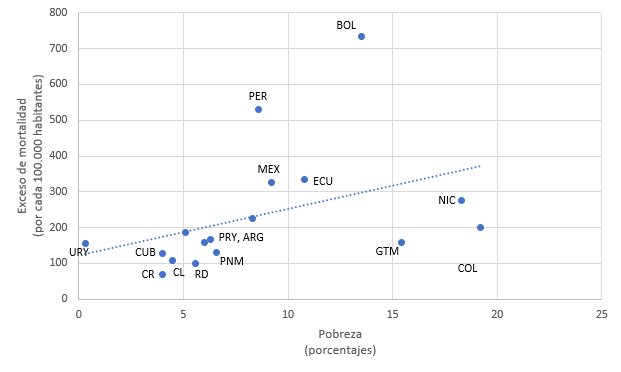 Source: Prepared by the authors, on the basis of Institute for Health Metrics and Evaluation (IHME), COVID-19 Excess Mortality Estimates 2020-2021 [online database] https://ghdx.healthdata.org/record/ihme-data/covid_19_excess_mortality, and Economic Commission for Latin America and the Caribbean (ECLAC), CEPALSTAT [online database] https://statistics.cepal.org/portal/cepalstat/index.html?lang=en.
Source: Prepared by the authors, on the basis of Institute for Health Metrics and Evaluation (IHME), COVID-19 Excess Mortality Estimates 2020-2021 [online database] https://ghdx.healthdata.org/record/ihme-data/covid_19_excess_mortality, and Economic Commission for Latin America and the Caribbean (ECLAC), CEPALSTAT [online database] https://statistics.cepal.org/portal/cepalstat/index.html?lang=en.
a The countries included are: Argentina, Brazil, Chile, Colombia, Costa Rica, Cuba, the Dominican Republic, Ecuador, El Salvador, Guatemala, Mexico, Nicaragua, Panama, Paraguay, Peru, the Plurinational State of Bolivia and Uruguay.
Towards comprehensive, sustainable and resilient health systems
The impacts of the pandemic on socioeconomic dimensions, such as increased poverty and the effect on household income and the labour market, are expected to worsen the unequal distribution of the social determinants of health, deepening inequalities in the region. This situation is all the more worrisome considering the profound impact the pandemic has had on health systems. This points to the need to move towards universal health systems that guarantee access and ensure that people's basic needs are met, regardless of their employment status.
While recognizing the consequences of the crisis on the health system (displacement effect, build-up of demand for non-COVID-19 pathologies and duplicated demand), the countries stress the need to continue tackling the pandemic through the primary health care system, public health measures and the deployment of vaccination. The document describes how, during the first year of the pandemic, policy on health financing responded in the right direction, but was not sufficient or adequately sustainable and varied greatly between countries. Despite increased public spending and a reorganization of services, problems of access and low financial protection could not be avoided. This produced major health impacts measured in the form of excess deaths. Increasing public spending on health is key to addressing the structural changes required to build stronger resilience to future crises.
Seven lessons learned from the pandemic
Initially, measures to contain the spread of the virus in the region consisted exclusively of lockdowns, social distancing and the use of personal protective equipment, together with cash support to help the population to comply with these measures. During the second year of the pandemic, vaccination against COVID-19 became the main health tool. The slow and uneven progress of the vaccination process in the region indicates that regional cooperation and coordination mechanisms need to be strengthened.
Seven lessons may be drawn from the analysis of how the pandemic evolved and the vulnerabilities and strengths of health systems and their determinants in the region:
- Health is central to inclusive, economic and sustainable social development.
- Health policies must be comprehensive in nature, given that the social, economic and environmental dimensions are profoundly interdependent.
- The inequality that has marked the vaccination process highlights the importance of regional cooperation and coordination and international collaboration.
- The region’s health systems urgently need to be restructured towards universality.
- Health systems must move towards financial sustainability and public spending needs to be increased on the basis of a new fiscal compact.
- The reorganization of health services into integrated networks and primary care should be the main target of the new resources.
- Health systems need to be made more resilient and services brought closer to the population, with the capacity to reach out into the community.